CARDIOVASCULAR DISEASE
Cardiovascular disease is the leading cause of death worldwide for both men and women. The good news is that we have a profound understanding of the disease and how it progresses. The bad news is that many providers do not take advantage of the available resources, leaving patients wondering how they could possibly have had a cardiovascular event. This page will dive into the staggering numbers related to cardiovascular disease and how common it is. We will also discuss risk factors, both modifiable and non-modifiable, and why you should be paying very close attention to these. You may have never heard of some of the risk factors discussed, but you will be glad to have learned about them. We will discuss blood biomarkers as well as diagnostic tests, symptoms and the precise mechanism for the cause of cardiovascular disease. We will end with a discussion on prevention, focusing on strategies to modify the modifiable risk factors.
NOTE: Cardiovascular disease (CVD) encompasses disease of the coronary arteries, peripheral (arms and legs) arteries and cerebral (brain, associated with stroke) arteries. I will broadly refer to disease as CVD throughout.
Jump to:
OVERVIEW
CVD is the world's leading killer. That is bad news. The good news is that we know an awful lot about how it takes hold, how it progresses and what the major risk factors are that trigger it. But now for some more bad news. Most people are not doing the right things to prevent this disease from taking hold. This is not the fault of the average person, it is merely an effect of both a system that is designed to treat disease, not prevent it, and a society that is built to promote CVD progression (unhealthy food choices, lack of activity, etc.). There is no singular "pill" to prevent heart disease. A multi-faceted and complex approach must be taken to each individual's situation in order to design a strategy to combat the disease. I would argue that doing everything in your power to avoid becoming another number in the dreadful CVD death statistics is paramount if you intend to live a healthy, meaningful life into old age. And my main argument is that you should start now, not when you are "sick."
By the Numbers
Cardiovascular disease (CVD) is the number one killer globally, that is for men, women and people of all races. According to the World Health Organization, 17.9 million people died from CVD in 2019. That is, roughly 1/3 deaths were due to CVD, and the bulk (85%) of those were due to heart attack and stroke.
805,000 people have a heart attack every year and about 200,000 of those heart attacks happen to people who have already had one. Thankfully, due to incredible advancements in medical technology and health care, about 95% of those having a heart attack will survive their hospital stay, assuming they get to the hospital in a timely manner.
Unfortunately, surviving that initial hospitalization is only half the battle. Data shows that those who have a heart attack are at an increased risk of having a repeat Major Adverse Cardiac Event (MACE, generally defined as another heart attack, stroke or death) in the first year (18.3% chance) and continue to remain at high-risk long-term (20% chance of MACE at 3 years). Another systematic review of studies showed that individuals having a heart attack more than 1 year in the past still had a 30% higher chance of having an adverse cardiac outcome (another heart attack or death) both 1-3 years or 3-5 years post initial heart attack.
There is another piece of information worth considering. At this point, you might be thinking "Well, of course these people are having heart attacks and dying. They're old!" But that is not exactly true.
A study done in the United States suggests that roughly 50% of all new-onset cardiovascular event will occur before the age of 65 in men, and about 33% will occur before the age of 65 in women.
Additionally, 1/5 deaths for individuals aged 25-64 could still be attributed to heart disease in 2017.
And a study done in Brazil shows the long-term outcomes for these younger individuals aren't great. It evaluated long-term survival of patients undergoing "percutaneous coronary intervention" (meaning, they had a coronary artery with a plaque build-up that was 'opened up' by procedure. They did not necessarily have a heart attack). In just looking at the patients in the age group from age 20-49 (about 3,000 patients over 11 years), here is what survival looked like over time.
-
One Day: ~99%
-
1 year: ~96%
-
5 years: ~89%
-
10 years: ~79%
-
15 years: ~69%
In other words, this data suggests that individuals having their first heart attack (or coronary procedure) before the age of 50 years old have about a 30% chance of dying in 15 years. Combined with other available data, we have a nasty recipe. Unsuspecting individuals under the age of 65 are at serious risk for heart attacks and other cardiac complications, and these issues are associated with a very poor outlook and quality of life.
What is not captured here, but surely you can imagine, is the reduction in quality of life for those that have survived a heart attack. A heart attack generally leads to reduced physical capacity and therefore an inability to partake in previously enjoyable activities, there is increased anxiety due to the fear of a recurrent episode and there are typically other health conditions a patient having experienced a heart attack is managing, which is obviously not something desirable.
Heart disease is the number one killer in the world, and it afflicts people of all genders, races and ages. As is hopefully already obvious, but will certainly become clearer, it is never a bad idea to start thinking about your own heart health.
Types of Prevention
-
Primordial Prevention: Preventing the development of risk factors (high blood pressure, high cholesterol, etc.) for CVD.
-
Primary Prevention: Treatment of adverse levels of risk factors for CVD
-
Secondary Prevention: Preventing the recurrence of clinical events (heart attacks, stroke, etc.) in those with diagnosed CVD.
Regardless of which bucket you fall in, there is no time like the present to understand your risk factors and to start addressing them. If you go for an annual check-up, you may be told you have nothing to worry about. But you must understand what was evaluated at that check-up to come to that conclusion.
The key is to understand YOUR goals. I am sure your goal goes beyond not having a heart attack in the next, say 5-10 years. You would probably like to NEVER have a heart attack. Below we will discuss risk factors, biomarkers, and diagnostic tests you should become familiar with to reduce your lifetime risk of heart disease and the deterioration of quality of life associated with it.
Causes and Pathology
Below will outline the literal steps in the progression of how cardiovascular disease occurs. It is vital to understand this process. It will become apparent why the known "risk factors" are just that, risk factors for the development and progression of this disease process. (Note: this is not a comprehensive review, but a general overview.)
-
Early in life, cholesterol (specifically, LDL particles) begins to deposit in the artery walls, specifically in the "subendothelial space".
-
This process is normal, but can progress and lead to CVD
-
If the LDL particles are oxidized due to exposure to reactive oxygen species, the cascade of CVD is kicked off
-
These oxidized LDL particles trigger the artery to initiate an inflammatory/immune response, because the oxidized particles are toxic to the artery (the endothelium).
-
In response, a particle known as a "monocyte" is sent to the artery to address the oxidized particle
-
The monocyte enters the subendothelial space and devours the oxidized LDL particles (at this point, the monocyte is called a macrophage)
-
The macrophage then transforms into a "foam cell" due to the ingestion of the LDL particles
-
Macrophages grow larger as they absorb each other and they further damage the artery and endothelium
-
This continued damage triggers the immune system to "patch up" the damaged areas of the endothelium which results in the formation of a fibrous cap over the foam cell (aka fatty streak because this fat rich cluster appears as an initial sign of CVD). We would call this "plaque."
-
At this point, the artery is now beginning to show signs of narrowing (note, up to this point, none of this would be "diagnosed" with standard physical exam or diagnostic testing)
-
This plaque is primarily made up of fat and is therefore soft. The plaque can continue to accumulate and, over time, result in a "blockage" that can lead to symptoms of heart disease (symptoms can show up when the artery is about ~70% blocked)
-
If the plaque blocks the artery 100%, there is no blood flow the heart beyond the blockage, and one would have a heart attack
-
More commonly, before the plaque blocks the artery 100%, it can "rupture" because it is soft.
-
When a plaque ruptures, it triggers a clotting response and that piece of plaque is quickly hit by platelets, fibrinogen, etc. and turns into a clot.
-
This clot will then block an artery leading to a heart attack (note: most heart attacks are caused by this plaque rupture and clotting, not by a 100% blockage. Even with a small plaque build-up, the rupture is possible, which is why it is so important to do everything we can to prevent the plaque from forming)
-
Calcium is one of the final products of plaque formation. This process ultimately hardens the plaque, leaving it less susceptible to rupture. This is what we look at with a Coronary Calcium test, and hopefully you realize how a positive calcium test is very late in the progression.
Take Home Point
Cardiovascular disease is a complex, systemic disease, but thankfully we have a solid grasp of what causes the disease and how it progresses. Because of this, we can better treat and prevent it.
Based on what is described above, we can paint a clear picture of what triggers can lead to the progression of heart disease. Primarily, those triggers would be:
-
LDL-Particle Number: Distinct from cholesterol, as will be described in another section, a high level of LDL particles increases the likelihood that an LDL particle will deposit in an artery, therefore increasing the likelihood that an LDL particle in the endothelium could be oxidized, starting the process.
-
Endothelial Dysfunction: Anything that can damage the endothelium will increase the likelihood of depositing LDL particles in the endothelium. This dysfunction also leads to artery stiffening and a number of other consequences that increaes CVD risk
-
Inflammation: Chronic inflammation is a bad sign for heart disease because, as we described, the inflammatory response to oxidized LDL particles can lead to artery narrowing and plaque development. But inflammation is also a causal factor, meaning that chronic inflammation can also directly impact the amount of LDL particles being deposited in the artery. It is important to manage chronic inflammation, which means identifying the cause (plaque in the arteries, metabolic disease, stress, smoking to name a few) and reducing the inflammatory response.
Anything one can do to reduce LDL particle number, improve endothelial function and reduce inflammation will go a long way in preventing CVD. Now that we understand what causes CVD and the specific triggers associated with its progression, we can look at the risk factors that fuel the triggers.
Risk Factors
There are certain "triggers" for the cause and progression of heart disease, as mentioned above. These triggers are fueled by specific factors that increase the risk of developing cardiovascular disease. Therefore, it is important to understand these risk factors and to get them under control before disease has taken hold. Here, we will discuss "modifiable" risk factors, meaning those that can be impacted by lifestyle changes or prescription drugs. There are also "non-modifiable" risk factors like gender and age.
ApoB
ApoB concentration is the biggest risk for heart disease you have never heard of. This is a blood test that should be requested of the doctor if it is not already ordered. This lab value provides us the number of atherogenic (CVD causing) particles in the blood, which is ultimately what we care about. What was outlined above explains that the number of LDL particles, not the amount of LDL cholesterol, drives CVD risk. The difference is subtle in nomenclature, but not in risk.
Lp(a)
A quick note on Lp(a). This is a distinct lipoprotein that is similar to LDL particles but results in a disproportionatlyy higher risk of CVD. Lp(a) (pronounced 'L-P-little-A') concentration is driven by genetics and high levels are present in roughly 1/5 to 1/10 individuals. High levels of Lp(a) independently increase CVD risk so you have to know this number, and it only needs to be checked once in your life (it is driven by genetics)! This is yet another variable that can account for the "I did everything right, how do I have heart disease" person.
Blood Pressure
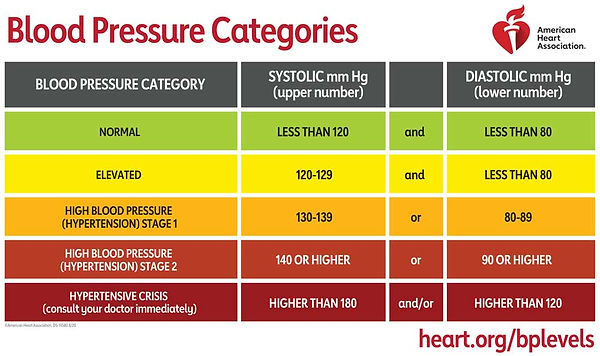
Elevated and high blood pressure (known as hypertension) is a major risk factor for heart disease. The reason is that the high-pressure results in turbulent blood flow in the arteries. This turbulent flow can lead to damaged epithelium and even chronic inflammation, which you will recognize as two of our triggers for CVD. The blood pressure guidelines are as follows:
Notice the "and" and "or" statements in the 3rd column. The values above define normal versus high blood pressure. What is so important to point out is that this is not based on the 1 reading per year many of us are limited to at our annual doctors visit. To get a true understanding of your blood pressure, you have to take matters into your own hands. You should be gathering this data at home using an automated blood pressure cuff in order to get a more accurate picture of your blood pressure.
Physical Inactivity and Sedentary Behavior
This is the new smoking. It is abundantly clear that being inactive is dangerous. This kind of lifestyle predisposes people to increased risk of many diseases, but heart disease is near the top of the list. Exercise is known to improve blood pressure and endothelial function which are both important in keeping heart disease risk low. The fitter a person is, the lower their risk of developing CVD.
The current recommendation is for adults to participate in 150-300 minutes of moderate intensity physical activity or 75 minutes of vigorous activity, where moderate intensity activity is as simple as brisk walking or yard work and vigorous activity is something like running or cycling up and down hills. Individuals who do not meet these goals are considered physically inactive. Sedentary behavior is defined as "any waking behavior characterized by an energy expenditure ≤1.5 metabolic equivalents of task (METs), while in a seated, reclined or lying posture," or too much sitting and lying down. Physical inactivity and sedentary behavior both increase CVD risk, but what is scary is that even individuals that meet the activity recommendations (and therefore are NOT physically inactive) can washout some of the benefit of exercise by spending too much of their non-exercise time being sedentary. Picture a situation where one wakes up, exercises for one hour every morning, and then commutes to work for one hour. Sits at a desk for 8 hours. Drives home for another hour. Sits down for dinner, lays on the couch for TV and then goes to sleep. 1 hour of daily exercise and the rest of the hours being sedentary is not ideal for optimal health.
The American Heart Association released a Science Advisory back in 2016 that outlined much of the existing data in support of the idea that sedentary behavior was associated with CVD risk and death due to CVD. The evidence is overwhelming and points to a causal relationship between sitting too much and dying of heart disease. Although data exist suggesting that regular exercise can offset the risks of prolonged sitting, This particular meta-analysis showed that compared to a baseline group that spent <4 hours/day sitting and were in the most active group (~60 mins/day), those who sat for >8 hours/day and exercised the least were 59% more likely to die during follow up. However, those is the group that exercised the most AND sat the most, there was no increased risk of dying during follow-up. Interesting, yes, but to me it is still not worth the risk. So get up and move throughout the day!
With all of this said, and granting the fact that being active will improve health (more on this elsewhere), even the fittest person in the world cannot protect themselves from elevated levels of ApoB or Lp(a). This is why it is so important to have a full picture of your risk profile.
Metabolic Dysfunction
Diabetes and metabolic disease increase the risk of heart disease through several mechanisms. Directly, poor metabolic health can lead to "cardiometabolic" disease, which is a change in blood lipids that leads to increased levels of ApoB. As discussed elsewhere, metabolic disease leads to liver dysfunction that results in increased triglycerides and reduces HDL-cholesterol and can lead to increased LDL-cholesterol. Aside from this direct effect on blood lipid levels, metabolic dysfunction causes vascular damage to the epithelium and can result in chronic inflammation, both of which increase risk for heart disease. When being evaluated for heart disease risk, understanding metabolic health is foundational in the risk assessment.
Inflammation
Inflammation is quite abstract. There is not a single biomarker to look at, nor is there a biomarker that specifically confers risk of heart disease. With that said, here are a few biomarkers related to inflammation that you should consider asking about the next time you have blood work:
-
Homocysteine
-
hsCRP
-
Fibrinogen
Stress
High levels of stress can be a root cause issue that lead to a cascade of negative responses in the body. Mental health plays an important role in heart health as chronic stress can directly impact metabolic function, blood pressure and other triggers that can lead to the development of CVD. Stress can come in many forms. Whether it is related to work, relationships, home life, deadlines or anything else, the answer is not living a life free of stressors, rather, it is about developing the skills and coping strategies to mitigate the negative consequences of stressful circumstances.
Poor Sleep
Chronic, inadequate sleep quantity (how much) and quality (how well) is a major risk factor for CVD that is underappreciated. The result of poor sleep is similar to being in a high-stress or high-anxiety state. Our body is unable to fully recover, leading to an increase in our stress hormones and stress response. We simply stay in "fight or flight" mode, and cannot shift into "rest and digest" mode. This state is effectively both adding logs to the CVD fire while fanning the flames. The effects of poor sleep include elevated blood pressure and metabolic dysfunction, among others, which contribute to CVD risk. Adults should be aiming for a minimum of 7 hours, up to 9 hours of sleep each night. Given the ubiquity of wearable health devices and sleep tracking devices, it would be prudent to try one out and see how high the quality of sleep is.
Smoking
Honestly, not too much to say on this one. Smoking increases the risk of CVD among a myriad of other health conditions. If you are a smoker, you should quit, but you already know this. Smoking can flare up all of the triggers of heart disease, and it can independently cause increases in blood pressure, endothelial damage and more bad stuff!
Symptoms
Roughly 1/3 of patients' first "symptom" of cardiovascular disease is that they have a heart attack and DIE. That means one day, an individual is "free" of heart disease, and the next day they have a heart attack and dies. 2/3 will present in a different way and then begin treatment. So, the question is, are there symptoms a patient might have BEFORE the heart attack so they can get started on PREVENTING the heart attack from happening in the first place. The answer is technically yes, but once you have symptoms, the disease is very far into its progression.
We obviously argue that a person doesn't suddenly have CVD once they show symptoms or have a major adverse cardiac event like a heart attack. Nonetheless, many of us, despite our best efforts, will end up with advanced CVD and understanding symptoms can be life-saving.
Angina: This is the classical sign of restricted blood flow to the heart. It often is associated with a heart attack but can be experienced intermittently with exertion and go away with rest. This is a sign that the blood supply to the heart is restricted by a plaque build-up.
-
Chest tightness/pressure
-
Pain that radiates to the arms, neck, jaw or back
-
Pressing, squeezing or crushing pain
-
In women, it can present as indigestion or heart burn
Shortness of Breath
Fatigue
Pain, numbness, weakness or coldness in the arms or legs
Swelling in the legs or ankles
Fast or Irregular Heartbeats
Pounding or Racing Heart
General Weakness
As you can tell from this list of symptoms, they are very non-specific. This means that these symptoms could be signs of issues that are unrelated to CVD. They still warrant ruling it out, but they don't automatically confirm its presence. Angina is the only specific symptom but is often a very odd and hard to explain sensation. Many people don't realize they are having it. It is most evident during exertion, and then it goes away with rest, so often it is ignored, that is until it doesn't go away. Also, women do not experience angina the same way as men, making it even more non-specific and therefore more difficult to diagnose.
Diagnosis
Below is a brief overview of common diagnostic tests for cardiovascular disease. It is not meant to be exhaustive. Also, these tests would be ordered by a certified healthcare professional. Which test is right for which person, and which tests will get covered by insurance, are questions that must be answered at an individual level.
Non-Invasive Tests
Exercise (or Pharmacologic) Stress Test
The "Stress Test" is meant to challenge the heart, forcing the need to increase blood supply. Whether achieved through exercise or a drug that causes and increase in heart rate, the end goal is the same. The challenge can uncover abnormalities of the heart visible through an electrocardiogram (EKG/ECG). Certain abnormalities are an indication that the blood flow to the heart is inadequate. This test can be run in someone who is symptomatic or asymptomatic, but the symptomatic individual is much more likely to have a positive test. Remember, they are likely experiencing angina with exertion, which is caused by reduced blood flow to the heart. A positive stress test (ECG abnormalities identified) would lead to further, likely invasive, testing as stress tests are not 100% accurate, meaning there can be "false positives" which must be addressed with more specific testing.
Coronary Artery Calcium (CAC) Score
This is a test that requires a simple CT scan of the heart. This scan can identify if there is any calcification in, and therefore narrowing of, the arteries of the heart and is reported in a score ranging from 0 to over 1000. A score of 0 indicates there is no calcified plaque in the coronary artery, and the higher the score, the more calcified plaque there is. Higher scores indicate higher risk for major adverse cardiac events. This is valuable information, but is not totally informative, particularly in younger patients. Calcification of plaque is an end-stage process in CVD progression, so if you are a "younger" individual and have a non-zero score, this is something to be concerned with.
The test is not without limitation in that it can sometimes give an individual a score of zero, when in fact they have a non-zero score. Additionally, when we discuss "risk" in the context of the CAC score, we are talking about 10 year risk (as seen in this calculator). We don't have any information about risk beyond that, and in younger folks we likely want to concern ourselves with the risk over the longer term. This is a useful tool, but it is not the perfect tool.
CT Angiogram
Like a Coronary Artery Calcium Score, this test is looking to identify any narrowing of the coronary artery. Typically, the test will go like this. A baseline CT scan of the heart is completed to identify any calcification (just like in a CAC). Then, contrast is injected into the patient and another CT scan is completed. The contrast will eventually make its way through the blood stream to the heart. The CT scan will capture an image of the heart with the contrast visible in the coronary arteries, and this visualization can identify any non-calcified plaque, or soft plaque, that is causing a narrowing of the arteries.
This is a better test than the CAC score because it can identify soft plaque which is invisible in the CAC score. This is not to say that everyone should have a CT angiogram. The test can be cost prohibitive if not covered by insurance and it does come with risks that should be weighed in a conversation with a healthcare professional.
Invasive Tests
Cardiac Catheterization and Coronary Angiogram
This test requires a trip to the hospital and the "cardiac catheterization laboratory." A physician will insert a small tube, known as a catheter, into a blood vessel in either the arm or groin. Once the catheter is in the blood vessel, it is guided through the vasculature to the heart. At this point, contrast can be injected through the tube and x-ray can be taken simultaneously to visualize any blockages or plaques in the coronary artery. This sounds much like the CT angiogram in terms of end result, but the means to get the images are different.
This test certainly provides great imaging and a great idea of how advances CVD is, but it is generally reserved for individuals experiencing debilitating symptoms, or even those who have had a major adverse cardiac event. Again, a healthcare provider would weigh the risks and benefits of an invasive test like this and decide if it is the correct action at the individual level.
Management
Prevention of cardiovascular disease should really be viewed as treatment. Ultimately, we are trying to prevent the adverse cardiac events (heart attack, stroke, etc.) as opposed to preventing any manifestation of CVD. We will all develop some degree of CVD, the goal is to not let it kill us. Therefore, prevention of major adverse cardiac events starts with the treatment of CVD risk factors.
This is where you must Compete to Live. Here are some of the best tools at our disposal for the treatment and management of CVD risk factors:
-
Open Communication with Health Care Providers: It is imperative to be comfortable having a conversation with HCPs. One must be comfortable not only discussing long-term health goals, but also comfortable discussing tests that may or may not be helpful given the individual situation. This is often overlooked but is fundamentally critical to disease prevention. Clear goals and a clear understanding of the barriers to accomplishing those goals set the stage for the necessary actions to preserve health.
-
Apo-B Management: One must know this number. Apo-B must be run when blood work is done, and one must know how to interpret and manage the results
-
Lp(a): One must know if this genetically driven risk factor is present. It should be run once to understand risk
-
Blood Pressure Management: One must know what their blood pressure is. This is not the blood pressure you get once a year at an annual visit. This is going to take some effort to measure independently, at home.
-
Exercise: Avoiding long periods of daily sitting can prevent some of the negative effects of sedentary behaviors on the body and the vascular system. Regular exercise can improve the function of the vascular system. Don't sit. Be active. Double the benefit.
-
Metabolic Health Management: Diabetes and metabolic disease can lay the foundation for progression of CVD. Our body is a complex system of interconnected and interacting parts. It is important not to treat each part independent of the others.
-
Smoking: Don't do it!